To set the stage a bit we have been discussing with Keith’s doctors the options for follow-up treatment now that he has completed the usual protocol for his type of cancer and staging. With a clean series of current tests showing no evidence of disease (NED) or minimal residual disease (MRD) the standard of care is to administer a drug called 13-cis-RA or high dose vitamin A that is primarily used in cancer treatment to mop up the few lingering tumor cells that could still be lurking about. This treatment would last for approximately 6 months but is easily administered at home with a pill and under such a plan Keith could pretty much go about gradually resuming normal activities.
So to complete the overall picture and bring you up to date, Keith finished the usual series of standard ‘work-up’ tests beginning on the 17th through the 23rd of May and these diagnostics included a bone scan, a CT scan, a heart echo, a pulmonary function test, a MIBG scan, and a pelvic bone marrow aspirate & biopsy. The results of all these tests looked encouraging – that is all except one. The MIBG suggested that there were a couple of ‘hot spots’ that were cause for concern and required additional testing. So last Friday Keith returned to Stanford to have an MRI scan. We learned yesterday that the results of MRI seem to confirm the MIBG finding which is to say that his cancer apparently either has not cleared completely or has relapsed.
If you are a glutton for medical terminology punishment this link to the study brief should do the trick: COG-ANBL0322. As I understand it the basic approach here is to introduce a special monoclonal antibody that is designed to seek out and bond to neural cells and specifically neuroblastoma tumor cells, tagging them in a way that allows the body’s own immune system, enhanced by Interleukin-2 to destroy these cells. Despite the sometimes difficult and frankly unknown side effects of this regimen, it seems to us like the best possible course for Keith right now. This effectively means months of additional treatment with regular inpatient stays at the hospital and many more tests – assuming he responds favorably to the treatment. We are not facing the moral dilemma we would have faced if Keith’s tests all came back clean – that is whether to have put Keith through the misery of a similar clinical trial or essentially to have done nothing and hoped we had done enough. No, the only choice here is to move on to the next treatment option.
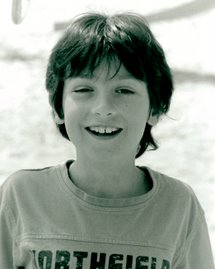
Of course it was a difficult conversation to have with Keith and didn’t take long for him to process the implications of this news. It would mean that the carefree days of summer that he had been anticipating and deserving of would probably not happen – at least not this year. His mind raced: What about school in the fall? What about my friends? What about just being normal again? He was angry at us, he was angry at the doctors, and at one point he simply stated that he’d had enough. No more. Enough.
It was a difficult moment for all of us and he of course was right to be upset. Still, after struggling with the severe disappointment of this news he soon composed himself, calmed himself down, processed the options, projected the outcomes and ultimately resigned himself to the necessity of more treatment.
With more guts and courage than I could ever muster Keith said “OK, Whatever. There doesn’t really seem to be a choice.”